
TMJ Disorders
Temporomandibular Joint (TMJ) Disorders are defined as chronic inflammation, pain or other symptoms related to injury, damage or improper alignment of the jaw joints.
Temporomandibular Joints (TMJ)
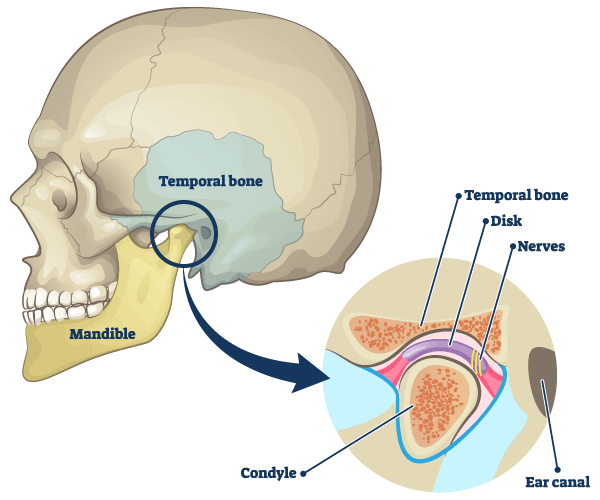
There is one TMJ on either side of your jaw. The temporomandibular joints (TMJ) form the connection between the temporal bone of the skull and the mandible (lower jaw). If you rest your fingers just in front of each ear and open and close your mouth, you will feel the TMJ in action.
How the TMJ works
The TMJ are considered to be among the hardest working joints in the body. They are used countless times per day to open/close the mouth, chew, speak or yawn.
Each end of the jaw bone (condyle) fits together with the temporal bone socket to form the temporomandibular joint; combined with the jaw muscles and cartilage, this allows the jaw to move in any direction:
- As the facial muscles move the jaw, a cartilage ‘articular’ disc serves as a soft, smooth buffer for the condyle to move forward and back within the socket to open/close the mouth (hinge) or slide the jaw from side to side.
- The TMJ disc is surrounded by synovial fluid sacs to cushion and protect the bones from damage during movement.
TMJ Disorder Symptoms
- Jaw
- Soreness
- Noises, clicking / grating
- Locking closed or open
- Ear
- Earache
- Dizziness or vertigo
- Ringing in ears
- Recurrent ear infections
- Headaches
- Shooting pain across back of head
- Pain in forehead / temples
- Migraines
- Cluster headaches
- Eyes
- Pain or pressure behind eyes
- Light sensitivity
- Blurred vision
- Mouth
- Limited opening
- Burning tongue
- Dry mouth
- Snoring
- Teeth
- Teeth grinding / bruxism at night
- Fractured or worn teeth
- Painful chewing
- Clenching
- Face, Neck & Shoulder
- Muscles / myofascial
- Back and shoulder pain
- Neck pain or limited movement
- Throat
- Chronic sore throat
- Difficulty in swallowing or tightness in throat
Athens dentist Dr. Phillip Durden discusses TMJ disorders and Sleep Apnea
What causes TMJ Disorders?
Diagnosing the cause of TMJ disorders can be complex, as symptoms are varied and issues related to the TMJ may actually be secondary symptoms of a primary illness.
TMJ pain or symptoms generally occur due to injury to the joint, arthritis or misalignment and dysfunction of the articular disc (temporomandibular dysfunction or TMD).
TMJ Injury
A blow to the jaw can damage the bones, muscles and cartilage that form the joint or shift the location of the articular disc.
If you can imagine how difficult it is to ‘rest’ the TMJ and refrain from chewing or talking, it is understandable that healing from injury or managing pain from a displaced TMJ disc can be challenging. Patients may have symptoms for months or even years after a TMJ injury.
Chronic teeth grinding (bruxism) or jaw clenching places added strain on facial and jaw muscles that can lead to pain and inflammation in the TMJ. Bruxism and clenching can also contribute to tooth fracture and bone loss in the jaw. Learn more about teeth bruxism and clenching.
Myofascial Pain and TMJ
A ‘trigger point’ of pain occurs when an area of muscle tissue becomes hyper-tense and sensitive due to strain, injury or overuse. The trigger point causes the pain to span the connective tissues (fascia) that cover the muscles and present as ‘referred pain’ in other muscles throughout the body, a condition known as myofascial pain syndrome. Trigger points can often be misleading in diagnosing TMJ disorders.
Persistent bruxism and jaw clenching is wearing on the muscles that connect the jaw to the skull; without treatment, this can result in trigger point pain that impacts the TMJ, face, neck and shoulders. Learn more about myofascial pain syndrome.
Arthritis
Arthritis is a common cause of joint problems throughout the body. In the TMJ, arthritis leads to bone degeneration and breakdown of the disc cartilage and synovial tissues. Without these protective coverings, the bones of the TMJ can grate on each other (‘bone on bone’) during movement, causing pain and inflammation within the joint and in the surrounding muscles.
The TMJ Disorder and Obstructive Sleep Apnea connection
Known as the ‘great imposter’, TMJ symptoms can actually be the result of obstructive sleep apnea (OSA), a disorder that causes the body to stop breathing multiple times during sleep.
As the OSA patient struggles to breathe, they may clench their jaw, grind their teeth or shift their jaw as the body attempts to re-open the airway. This overwork and strain on the TMJ can cause pain and symptoms that may initially conceal the actual sleep disorder diagnosis. Learn more about obstructive sleep apnea.
What treatment options are available?
Treatment for TMJ Disorders, or TMD, is primarily focused on alleviating pain and symptoms, as well as addressing the source of the problem.
Most people experience some type of temporary jaw pain on occasion related to yawning, gum chewing, poor posture or clenching in stressful situations. Mild, temporary jaw pain may resolve on its own with over the counter pain medication, stress reduction, muscle massage or ice packs.
Call Dental Sleep Medicine of Athens for TMJ Consultation
If you experience TMJ symptoms that last for more than a few days or are recurring, it may indicate a problem that requires further treatment. Please contact our office for an examination and consultation with Athens TMJ dentist Dr. Phillip Durden.
TMJ Consultation & Examination
During your TMJ consultation, Dr. Durden will talk with you about your dental and medical history to learn more about your overall health. He will combine this information with a thorough TMJ examination, including any necessary x-rays or imaging to evaluate TMJ function.
If Dr. Durden suspects internal damage to the TMJ or disc displacement, he may recommend MRI imaging and radiologist review to assess TMJ function and the health of the articular disc and surrounding synovial tissue.
TMJ and Bruxism
If your TMJ symptoms or disc displacement are related to nighttime teeth grinding (bruxism) or jaw clenching, Dr. Durden may recommend that you wear a removable oral appliance, or biteguard during sleep. The oral appliance (or nightguard) is worn over the teeth to create a cushioned buffer so that any potential harm from grinding the teeth or jaw clenching is prevented or minimized. Learn more about TMD oral appliance therapy.
TMD and Obstructive Sleep Apnea (OSA)
When TMJ symptoms are accompanied by heavy snoring, hypopnea symptoms or excessive daytime drowsiness, Dr. Durden will refer the patient to a sleep specialist for evaluation for possible sleep breathing disorders or obstructive sleep apnea (OSA). If a diagnosis of sleep breathing disorder is confirmed by the physician, Dr. Durden will work closely with the sleep specialist to support oral sleep appliance therapy if needed to assist with airway management. Learn more about OSA oral appliance therapy.
TMJ Surgery
Surgical treatment of TMD is uncommon and usually the last option considered. There are cases, however, when a physician may recommend surgery to remove bone or tissue growths or diseased areas of bone to restore TMJ health.
Dental Sleep Medicine of Athens
Athens TMJ dentist Dr. Phillip Durden has helped many patients find answers to unexplained headaches and facial pain related to TMJ/TMD.
If you are experiencing symptoms of jaw pain or know that you are grinding or clenching your teeth, please Contact Dental Sleep Medicine of Athens to schedule a consultation with Dr. Phillip Durden.