
Hypopnea
What is Hypopnea?
Hypopnea is slowed, shallow, restricted breathing that occurs in 10-second or longer ‘episodes’ repeatedly during sleep. Hypopnea episodes often occur along with sleep apnea events that cause the body to stop breathing completely for a few seconds until the brain tells it to wake up. A patient may endure a recurring cycle of hypopnea episodes followed by apnea events throughout the night.
If hypopnea is not treated, it can reduce vital air flow by 30-90%; this lowers the supply of oxygen to red blood cells and increases the risk of serious health problems. (sleepfoundation.org)
Like sleep apnea, hypopnea may be categorized as obstructive, central or mixed obstructive-central.
Obstructive Hypopnea
After we fall asleep, our brain and body fully relax. In cases of obstructive hypopnea, the relaxed muscles and tissues in the throat become slack and droopy, partially blocking the airway. The brain tells the body to continue the effort to breathe, however, the obstructed airway restricts proper air flow.
Loud, frequent snoring is a characteristic sign of obstructive hypopnea; the tissue blocking the airway vibrates and creates the ‘rattling’ sound of snoring as a limited amount of air passes through. (Not all people that snore have hypopnea, however; learn more about snoring.)
Central Hypopnea
Central hypopnea episodes are the result of a mechanical lack of effort to breathe vs. obstructed air flow. For central apnea patients, the brain does not send the body regular instructions to perform the action of breathing.
In contrast to obstructive hypopnea, snoring is not a symptom of central hypopnea. Central hypopnea may be linked to brain illness or injury, or medication use.
Mixed Hypopnea
Mixed hypopnea is used to describe combined obstructive and central hypopnea. Because mixed hypopnea involves both lack of respiratory effort and obstructed air flow, it is generally classified as a severe form of hypopnea.
What other health complications are associated with Hypopnea?
Restful sleep is essential for our mental and physical health. As we sleep, our brain refreshes to help us think more clearly and store memories. Virtually every body system takes care of important tasks while we sleep, such as cell growth for tissue healing and hormonal release to maintain immune health.
When the body is deprived of necessary sleep and is continually subjected to the effects of hypopnea (reduced air flow and lower blood oxygen levels), patients can develop a number of health problems, including:
- Morning headaches
- Inability to focus and lack of alertness
- Mood swings or depression
- Weight gain
- Sexual dysfunction
- Sleep incontinence
- Increased risk of diabetes, heart disease and stroke
What health conditions are linked to Hypopnea and Sleep Apnea?
Certain illnesses and health factors can increase a patient’s risk of developing hypopnea or sleep apnea:
- Smoking
- Obesity or large neck size
- Thyroid disease
- Muscular disorders
- Under-sized jaw structure
- Family history of hypopnea
- Gender (Men are more likely to have hypopnea than women.)
What treatment options are available for Hypopnea?
A medical sleep specialist is responsible for diagnosing hypopnea and will recommend treatment based on the type (central, obstructive or mixed) and the severity and frequency of hypopnea episodes.
Central Hypopnea Treatment
Because central hypopnea is the result of faulty brain signaling to the body, understanding the physical cause or underlying illness behind the hypopnea is crucial.
The sleep physician will first address the cause of central hypopnea with testing, diagnosis and treatment. It may be necessary to manage hypopnea symptoms with supportive therapy or lifestyle changes (as with obstructive hypopnea) in addition to treatment for the primary illness.
Obstructive Hypopnea Treatment
Like obstructive sleep apnea, treatment for obstructive hypopnea is centered on maintaining the airway for proper breathing during sleep. Common treatment recommendations for obstructive hypopnea include:
Lifestyle Changes and Weight Loss
Losing weight, reducing alcohol intake and quitting smoking can help improve the health and reduce inflammation of the tissues and muscles of the upper body and throat, helping to reduce or eliminate airway blockage while sleeping. In very mild hypopnea cases, lifestyle changes may be the only steps needed, or, in moderate to severe cases, appropriate life changes are recommended along with other treatments.
CPAP (Continuous Positive Airway Pressure)
CPAP is a small bedside machine that provides a continuous supply of gently pressurized air through a face mask that is worn during sleep. As the patient breathes, the steady flow of pressurized air from the CPAP system helps keep the tissue and muscle walls of the upper airway intact to allow air to pass through normally.
CPAP is a standard treatment for moderate to severe hypopnea and sleep apnea, however, not all patients can tolerate CPAP. Learn more about CPAP intolerance.
Surgery
Surgery for treatment of hypopnea is less common, although it is sometimes necessary. The sleep physician and surgeon may recommend removal, reduction or modification of nasal or throat soft tissue (as with tonsils or adenoids) to improve sleep health.
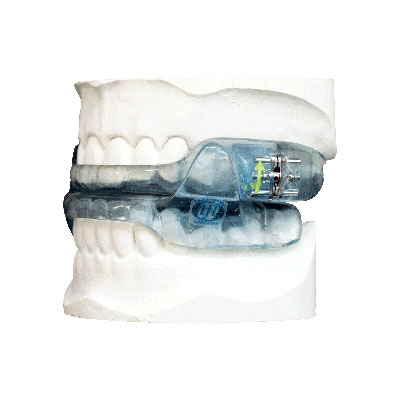
Image courtesy of True Function Laboratory
Oral Appliance Therapy
A sleep physician may prescribe oral appliance therapy in cases of mild to moderate hypopnea or sleep apnea, or for patients that are unable to tolerate CPAP. The patient is referred to a dentist that has completed advanced training in dental sleep medicine for the design and customization of a removable sleep appliance.
An oral sleep appliance is an FDA approved device; it is made of durable plastic and looks somewhat like a sports mouthguard. The device is custom designed to shift the lower jaw (mandible) into a position that helps the airway stay open during sleep. Learn more about oral appliance therapy.
Athens dentist Dr. Phillip Durden has over 30 years' experience and training in dental sleep medicine. Dr. Durden supports sleep physicians and patients with oral appliance therapy for treatment of hypopnea and CPAP intolerant sleep apnea at Dental Sleep Medicine of Athens.
Contact Dental Sleep Medicine of Athens
If your sleep physician has recommended oral appliance therapy for management of hypopnea or sleep apnea, we invite you to Contact Dental Sleep Medicine of Athens to schedule a new patient consultation with Dr. Phillip Durden.