
Obstructive Sleep Apnea
What is Obstructive Sleep Apnea?
Obstructive Sleep Apnea (OSA) is the most common form of sleep apnea, a health condition that causes the body to stop breathing repeatedly during sleep.
For most OSA patients, the apnea ‘event’ (breathing stopped) occurs multiple times per hour overnight.
Snoring & Obstructive Sleep Apnea
What are the Signs and Symptoms of Obstructive Sleep Apnea?
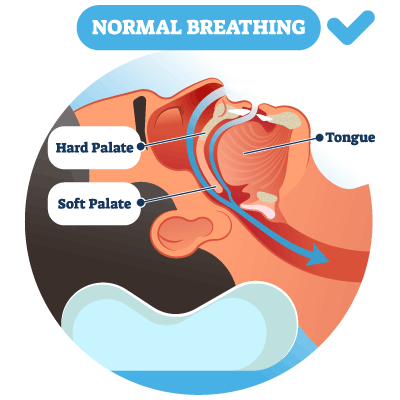
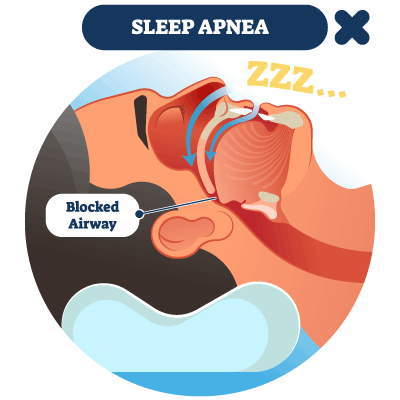
The most characteristic sign of OSA is chronic, loud snoring followed by choking or gasping sounds. As the loose soft tissues in the airway begin to sag and restrict air flow, a limited amount of air passes through and vibrates against the tissues to create the loud, raspy sound of snoring.
The snoring OSA patient will go silent briefly when the airway is fully obstructed and breathing stops, then wake up suddenly, gulping and choking for air.
- During deep sleep, all of our body muscles and tissues become fully relaxed.
- For OSA patients, as the body enters a relaxed state, the airway soft tissue structures sag and droop, obstructing the airway.
- When the airway becomes fully blocked, the patient stops breathing.
- As the brain detects that breathing has stopped, the patient wakes up gasping for air.
- Breathing again, the body falls back asleep (and the cycle repeats again).
Often, obstructive sleep apnea patients are not aware of how heavily they snore until a sleep partner tells them. The common belief is that ‘everybody snores’ - so, many patients live with undiagnosed OSA. Not all patients that snore have obstructive sleep apnea, however. Learn more about Snoring.
OSA Symptoms
Other signs and symptoms of OSA can be varied and do not always seem clearly connected to a sleep disorder. The OSA patient may just think they have trouble sleeping, or notice other symptoms and not realize they have a serious health problem.
Obstructive Sleep Apnea patients may experience:
- Morning headaches
- Dry, sore throat when waking up
- Difficulty concentrating
- Excessive daytime sleepiness
- Insomnia
- Sleep incontinence
- Depression
- Erectile dysfunction or loss of libido
Daytime Sleepiness & Drowsy Driving
Drowsy driving is a leading cause of injury and death in car accidents in the U.S. The CDC estimates that as many as 50,000 injuries and up to 6,000 deaths are linked with over 90,000 crashes related to falling asleep while driving (2017 data). Along with lack of sleep related to work and drowsiness from alcohol use or medications, sleep apnea is listed as a contributing cause of sleepy driving. (cdc.gov)
Take the Daytime Sleepiness Quiz
The Epworth Sleepiness Scale is used by sleep physicians in screening for sleep disorders. Please take this brief quiz to rate your level of daytime sleepiness and share your score with your primary care doctor.
How is Obstructive Sleep Apnea Diagnosed?
Obstructive sleep apnea is diagnosed by medical sleep professionals with a sleep study that is performed using sensor technology at a sleep testing facility. The study measures vital signs, breathing patterns, brain wave and muscle activity, eye movement and other diagnostic data while the patient sleeps (polysomnogram).
Portable home sleep study equipment may also be used by your doctor for screening or follow up testing. While not as detailed as a sleep study, home testing equipment tracks basic breathing and heart rates and oxygen saturation levels during sleep.
Learn more about Sleep Apnea Diagnosis.
Related Health Issues & OSA
A diagnosis of obstructive sleep apnea may be related to other health conditions:
- Obesity, smoking or alcohol use can impact breathing health, along with some drugs and medications.
- Major illnesses such as congestive heart failure, diabetes, asthma, previous stroke, high blood pressure, thyroid problems or hormonal disorders may be a contributing cause of obstructive sleep apnea or central sleep apnea.
- Patients with a family history of sleep-disordered breathing illness may be more likely to develop OSA.
- The risk of OSA increases with age, and men are statistically more likely to have OSA than women.
Learn more about Sleep Apnea.
TMJ/Bruxism & Obstructive Sleep Apnea
Known as the ‘great imposter’, temporomandibular joint disorder (jaw joint or TMJ) symptoms can initially seem to be limited to jaw joint function. Upon study by qualified medical professionals, OSA may be discovered as the underlying cause of TMJ problems.
Obstructive Sleep Apnea disguised as a TMJ Disorder
The jaw joints rely on proper sleep for healing and restoration, as does the rest of the body. When the body stops breathing during sleep, the entire body tenses up, including the muscles and tendons of the TMJ.
Jaw pain, neck and shoulder pain, and headaches that seemingly are related to TMJ disorders may actually be due to the lack of restful sleep and added strain placed on the TMJ. In these cases, TMJ problems are not truly jaw joint problems, but are actually hiding the real issue, obstructive sleep apnea. Learn more about TMJ disorders.
Teeth Grinding/Bruxism & Clenching
Research continues to reveal a high occurrence of sleep teeth grinding (bruxism) and clenching in OSA patients. One theory is that as the patient struggles to breathe, the throat and facial muscles tighten, creating added friction between the teeth and tension around the jaw joint.
The connection between bruxism/clenching and OSA is an area of continued study for physicians and dental sleep medicine professionals.
As a dentist trained in dental sleep medicine, Dr. Phillip Durden addresses bruxism and clenching symptoms as part of his overall analysis of TMJ disorders or OSA oral appliance therapy for CPAP intolerant patients.
What treatment options are available for Obstructive Sleep Apnea?
The primary goal of treatment of obstructive sleep apnea is to prevent airway restriction and impaired breathing (hypopnea) and blockage (OSA) to maintain healthy air flow and uninterrupted sleep. Sleep physicians may recommend a combination of common approaches to treatment for OSA:
Some patients with mild OSA may improve or eliminate symptoms by losing weight; this helps to reduce the amount of fatty tissue around the neck and relieve pressure on the airway.
Alcohol and sedative medications can have a depressant effect on the respiratory system. Avoiding these substances before sleep may improve or eliminate OSA symptoms.
CPAP (Continuous positive airway pressure) is the standard treatment for obstructive sleep apnea. The OSA patient wears a face mask while sleeping that is connected by tubing to a machine that produces a continual supply of mildly pressurized air. Breathing the pressurized air flow helps keep the airway soft tissues intact and reduce the risk of blockage.
Dr. Phillip Durden provides oral appliance therapy for OSA patients that are CPAP intolerant due to difficulty falling asleep, sinus irritation or other side effects. A removable OSA oral appliance is designed to position the jaw forward to assist with maintaining an open airway during sleep.
Surgery for treatment of obstructive sleep apnea is less common, but a sleep specialist may recommend removal of tonsils, adenoids or other sections of soft tissue to keep them from obstructing the airway during sleep.
Learn more about Sleep Apnea Treatment Options.
Health Complications from Obstructive Sleep Apnea
Obstructive sleep apnea reduces the oxygen supply to the body and diminishes much needed rest for the brain and the systems of the body. Untreated OSA can lead to severe illness, including heart disease, high blood pressure, diabetes or liver problems.
If you snore heavily and have been told that you snort and gasp for air during sleep, you should report these symptoms to your primary care physician and ask about obstructive sleep apnea. Treatment could be life-changing and potentially life-saving.
Dental Sleep Medicine of Athens
Dr. Phillip Durden provides oral appliance therapy for treatment of obstructive sleep apnea as directed by medical sleep specialists. If you have received a referral from a sleep physician or have questions about OSA, please contact the Dental Sleep Medicine of Athens team to get started on your path to healthier sleep today.
Read Dr. Phillip Durden's Article:
Headaches: Sleep Apnea and the Oral Connection .pdf
published in Southern Distinction Magazine